The Beck Depression Inventory (BDI) is a widely recognized and extensively used self-report questionnaire designed to assess the severity of depressive symptoms in individuals. Developed by psychiatrist Aaron T. Beck and his colleagues, the BDI has become a cornerstone in the field of mental health assessment, particularly for diagnosing and monitoring depression. Its simplicity, ease of administration, and robust psychometric properties have contributed to its enduring popularity among clinicians, researchers, and mental health professionals worldwide.
The BDI is not a diagnostic tool in itself, meaning it doesn’t definitively diagnose depression. Instead, it provides a quantitative measure of the intensity of depressive symptoms experienced by an individual over a specific period, typically the past two weeks. This allows for a more objective evaluation of a person’s emotional state, facilitating informed clinical decision-making and tracking the effectiveness of therapeutic interventions. Understanding what the BDI is, how it works, and its various applications is crucial for anyone involved in mental health care or seeking to gain insight into the experience of depression.
The Genesis and Evolution of the Beck Depression Inventory
The development of the Beck Depression Inventory was rooted in Aaron T. Beck’s cognitive theory of depression. Beck observed that individuals experiencing depression often exhibited characteristic negative thought patterns, or cognitive distortions, about themselves, their experiences, and their future. He theorized that these negative thoughts were not merely a consequence of depression but a significant contributing factor to its onset and maintenance. This cognitive perspective led to the development of the Cognitive Therapy for Depression, and the BDI was conceived as a tool to measure the cognitive and somatic symptoms associated with this condition.
Early Development and Theoretical Underpinnings
In the mid-20th century, psychiatric diagnosis often relied heavily on subjective clinical observation and symptom checklists that lacked precise standardization. Beck sought to create a more reliable and quantifiable method for assessing the multifaceted nature of depression. His early work involved identifying common themes in the self-talk of depressed patients, which he categorized into cognitive distortions. These included themes of hopelessness, worthlessness, self-blame, and pessimism. Alongside these cognitive elements, Beck also recognized the significant physical and emotional manifestations of depression, such as changes in sleep and appetite, fatigue, and a loss of interest or pleasure.
The initial version of the BDI, developed in the 1960s, was a 21-item multiple-choice questionnaire. Each item represented a specific symptom or attitude, and respondents were asked to select the statement that best described their experience. The statements were designed to capture a range of symptom severity, from mild to severe. This iterative process of identifying symptoms, formulating descriptive statements, and refining the instrument laid the groundwork for what would become a highly influential assessment tool.
Revisions and Refinements: BDI-IA and BDI-II
Over time, the BDI underwent several revisions to improve its accuracy, comprehensiveness, and alignment with evolving diagnostic criteria. The most significant revisions led to the creation of the Beck Depression Inventory-IA (BDI-IA) and, subsequently, the Beck Depression Inventory-II (BDI-II).
The BDI-IA, introduced in the 1970s, was an update that maintained the 21-item structure but incorporated some revisions to item wording and response options. This version aimed to enhance clarity and better differentiate between various levels of symptom severity.
The BDI-II, published in 1996, represented a more substantial overhaul. This revision was undertaken to align the inventory with the diagnostic criteria outlined in the third and fourth editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III and DSM-IV). A key change in the BDI-II was the removal of items related to suicidal ideation, which were considered to have sufficient overlap with anxiety symptoms and could be more appropriately assessed with dedicated instruments. Instead, the BDI-II introduced items reflecting feelings of worthlessness and self-hatred more prominently. It also modified items to better capture the core symptoms of depression as defined by the DSM. The BDI-II remains the most widely used version of the inventory today.
The evolution of the BDI reflects a commitment to scientific rigor and the continuous refinement of assessment tools based on empirical evidence and evolving clinical understanding of depression.
How the Beck Depression Inventory is Administered and Scored
The administration and scoring of the BDI are designed to be straightforward, allowing for efficient use in various clinical and research settings. The core of the inventory lies in its self-report format, where individuals respond to a series of statements reflecting their experiences over a defined period.
The Questionnaire Format and Symptom Domains
The BDI-II consists of 21 items, each with four response options representing increasing severity of a particular symptom or attitude. These items cover a broad spectrum of depressive experiences, broadly categorized into cognitive, affective, somatic, and vegetative domains.
- Cognitive Symptoms: These include items related to feelings of sadness, pessimism, guilt, disappointment, self-dislike, self-criticalness, indecisiveness, and thoughts of punishment.
- Affective Symptoms: This domain covers feelings of being a failure, loss of interest or pleasure, and irritability.
- Somatic Symptoms: Items in this category address changes in sleep patterns (insomnia or hypersomnia), changes in appetite (increased or decreased), fatigue or loss of energy, and physical complaints.
- Vegetative Symptoms: While not a distinct category in the BDI-II, some items, like changes in appetite and sleep, also fall under what are traditionally considered vegetative symptoms.

Each response option is assigned a score from 0 to 3, with higher scores indicating greater severity. For example, an item might have options like:
- 0: I do not feel sad.
- 1: I feel sad a good bit of the time.
- 2: I am sad all the time and I can’t snap out of it.
- 3: I am so sad or unhappy that I can’t stand it.
The administrator provides clear instructions to the respondent, emphasizing that they should choose the statement that best describes how they have been feeling for the past two weeks, including today. The time frame is crucial for ensuring that the responses reflect current symptomatic experience rather than a general disposition.
Scoring and Interpretation of Results
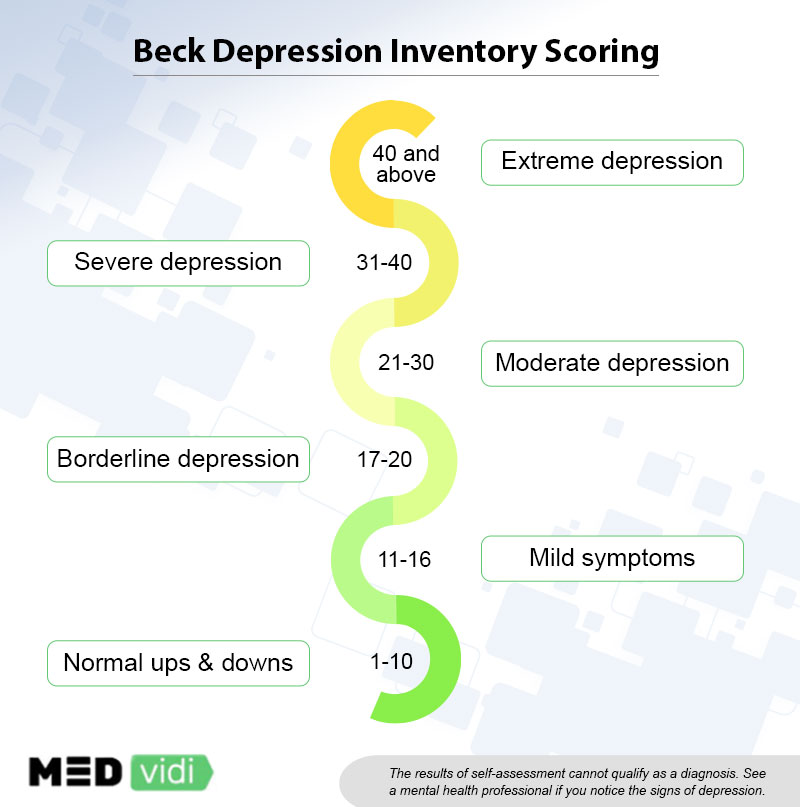
Once the respondent completes the questionnaire, the scores for each of the 21 items are summed to generate a total score. This total score then falls into one of several ranges, which are interpreted to indicate the severity of depressive symptoms. The generally accepted scoring ranges for the BDI-II are as follows:
- 0-13: Minimal Depression: Individuals in this range report very few or no depressive symptoms.
- 14-20: Mild Depression: This range suggests mild depressive symptoms that may be causing some distress but are unlikely to significantly impair daily functioning.
- 21-30: Moderate Depression: Individuals in this range are experiencing moderate depressive symptoms that are likely to be causing noticeable impairment in social, occupational, or other important areas of functioning.
- 31-40: Severe Depression: This range indicates severe depressive symptoms that are causing significant impairment and distress, and may warrant urgent clinical attention.
- 41-63: Extreme Depression: This range signifies extremely severe depressive symptoms, often associated with significant functional impairment and a high risk of suicidality, requiring immediate professional intervention.
It is vital to emphasize that these scores are intended for interpretation by qualified mental health professionals. The BDI is a screening and monitoring tool, and a score within a particular range does not negate the need for a comprehensive clinical assessment. Factors such as the individual’s history, current life circumstances, and other observable behaviors are essential for accurate diagnosis and treatment planning.
Applications and Limitations of the Beck Depression Inventory
The versatility of the Beck Depression Inventory has led to its widespread adoption across a variety of settings. Its ability to provide a quantifiable measure of depressive symptoms makes it invaluable for screening, diagnosis support, treatment monitoring, and research. However, like any assessment tool, the BDI has its limitations that are important to consider for responsible and effective use.
Clinical Utility and Research Applications
The primary application of the BDI is in clinical settings. Therapists, psychologists, psychiatrists, and counselors utilize the BDI to:
- Screen for Depression: It can be used as an initial screening tool to identify individuals who may be experiencing depressive symptoms and require further evaluation.
- Aid in Diagnosis: While not a standalone diagnostic instrument, the BDI scores can support a clinician’s diagnosis by providing objective data on symptom severity.
- Monitor Treatment Progress: One of the most significant benefits of the BDI is its utility in tracking the effectiveness of therapeutic interventions. Regular administration of the BDI can reveal whether a patient’s symptoms are improving, worsening, or remaining stable, allowing clinicians to adjust treatment plans accordingly.
- Identify Suicidal Risk: Although direct questions about suicidal ideation were removed in the BDI-II, the severity of scores, particularly in the higher ranges, can serve as an indicator for the need for a more in-depth assessment of suicide risk.
In research, the BDI has been instrumental in advancing our understanding of depression. It is used in:
- Epidemiological Studies: To assess the prevalence and incidence of depression in various populations.
- Clinical Trials: To evaluate the efficacy of new antidepressant medications and psychotherapies. Researchers can track changes in BDI scores in treatment groups compared to control groups to determine the impact of interventions.
- Investigating Correlates of Depression: Researchers use the BDI to explore the relationships between depression and other variables, such as personality traits, cognitive styles, and physiological markers.
Considerations and Limitations
Despite its widespread use and utility, it is essential to acknowledge the limitations of the Beck Depression Inventory:
- Self-Report Nature: The BDI relies on an individual’s self-awareness and willingness to accurately report their symptoms. Factors such as denial, social desirability bias, or a lack of insight can influence responses.
- Cultural and Linguistic Factors: While the BDI has been translated and validated in numerous languages, cultural nuances can sometimes affect symptom expression and interpretation. It is crucial to use culturally adapted versions and consider cultural context during interpretation.
- Symptom Overlap: Some symptoms measured by the BDI, such as fatigue, sleep disturbances, and appetite changes, can also be indicative of other medical or psychological conditions (e.g., thyroid problems, anxiety disorders). Therefore, a diagnosis should never be based solely on BDI scores.
- Limited Scope: The BDI focuses on core depressive symptoms. It may not fully capture the complexities of certain presentations of depression, such as atypical depression or depression in specific populations (e.g., children, adolescents, or individuals with psychotic features).
- Age Appropriateness: While the BDI-II is generally used for individuals aged 13 and older, specific versions or adaptations may be more suitable for younger populations.
- Not a Diagnostic Tool: As reiterated, the BDI is a measurement of symptom severity, not a diagnostic instrument. A formal diagnosis requires a comprehensive clinical interview and assessment by a qualified mental health professional.
In conclusion, the Beck Depression Inventory is a powerful and valuable tool for assessing depressive symptoms. Its continued relevance stems from its empirical grounding, ease of use, and adaptability. However, responsible application necessitates an understanding of its strengths and weaknesses, ensuring that it serves as a supportive component of a broader clinical and diagnostic process.
