The glycemic index (GI) is a ranking system for carbohydrate-containing foods based on how quickly they raise blood glucose levels after consumption. Understanding what constitutes a “good” glycemic index is crucial for managing blood sugar, improving energy levels, and promoting overall health. This guide will delve into the intricacies of the GI, its implications for different individuals, and practical advice for incorporating low-GI foods into your diet.
Understanding the Glycemic Index Scale
The GI scale ranges from 0 to 100, with pure glucose assigned a value of 100. Foods are categorized into three main groups based on their GI values:
Low Glycemic Index Foods (GI 55 or less)
Foods in this category are digested, absorbed, and metabolized slowly, causing a gradual and lower rise in blood glucose and insulin levels. This makes them an excellent choice for sustained energy release and blood sugar control. Examples include:
- Vegetables: Most non-starchy vegetables like leafy greens, broccoli, cauliflower, bell peppers, and tomatoes.
- Fruits: Berries, apples, pears, oranges, peaches, and plums.
- Legumes: Lentils, chickpeas, black beans, kidney beans, and soybeans.
- Whole Grains: Oats (steel-cut or rolled), barley, quinoa, and buckwheat.
- Dairy: Milk and yogurt (unsweetened).
- Nuts and Seeds: Almonds, walnuts, chia seeds, and flaxseeds.
Medium Glycemic Index Foods (GI 56-69)
These foods have a moderate impact on blood sugar levels. While not as beneficial as low-GI foods for steady energy, they can still be part of a healthy diet when consumed in moderation and paired with other low-GI options. Examples include:
- Certain Fruits: Bananas, mangoes, and grapes.
- Sweet Potatoes
- Brown Rice
- Whole Wheat Bread and Pasta
- Some Breakfast Cereals
High Glycemic Index Foods (GI 70 or more)
Foods in this category are rapidly digested, leading to a quick and significant spike in blood glucose and insulin levels. Frequent consumption of high-GI foods can contribute to energy crashes, increased hunger, and over the long term, an elevated risk of type 2 diabetes and other chronic health conditions. Examples include:
- Refined Grains: White bread, white rice, white pasta, and most breakfast cereals made from refined grains.
- Sugary Drinks: Sodas, fruit juices (especially those with added sugar), and energy drinks.
- Sweets and Desserts: Cakes, cookies, pastries, candy, and ice cream.
- Processed Snacks: Potato chips, crackers, and most packaged snack foods.
- Starchy Vegetables (prepared in certain ways): Mashed potatoes (especially instant), French fries, and cornflakes.
Factors Influencing a Food’s Glycemic Index
The GI of a food is not a fixed number and can be influenced by several factors. Understanding these variables can help individuals make informed food choices:
Processing and Refinement
The more a carbohydrate-rich food is processed or refined, the higher its GI tends to be. This is because processing often removes fiber and other nutrients that slow down digestion.
- Whole vs. Refined Grains: Whole grains like oats and barley retain their bran and germ, which are rich in fiber. This fiber slows down the digestion of carbohydrates, resulting in a lower GI. Refined grains, such as white flour, have had the bran and germ removed, leaving mainly the starchy endosperm, which is digested more quickly, leading to a higher GI. For example, steel-cut oats have a lower GI than instant oatmeal, and whole wheat bread generally has a lower GI than white bread.
- Whole Fruits vs. Juices: Whole fruits contain fiber that helps to moderate the absorption of sugars. When fruits are juiced, this fiber is largely removed, concentrating the sugars and leading to a faster rise in blood glucose. This is why a whole apple has a lower GI than apple juice.
- Minimally Processed Carbohydrates: Foods like sweet potatoes, legumes, and whole grains are generally considered lower GI options because their carbohydrate structure and fiber content slow down digestion.
Ripeness of Fruit
The GI of fruits can change as they ripen. As fruits mature, their starches are converted into sugars, which are more readily absorbed.
- Green Bananas vs. Ripe Bananas: A greener banana contains more resistant starch, which is not easily digested. As a banana ripens and turns yellow, this resistant starch converts to simple sugars, increasing its GI. Therefore, less ripe fruits generally have a lower GI than their fully ripe counterparts.
- Other Fruits: Similar effects can be observed in other fruits like avocados and even some starchy vegetables as they ripen.
Cooking Methods and Time
How a carbohydrate-rich food is prepared can significantly impact its GI.
- Al Dente Pasta: Pasta that is cooked “al dente” (firm to the bite) has a lower GI than pasta that is overcooked and mushy. Overcooking breaks down the starch molecules, making them easier to digest.
- Boiling vs. Baking Potatoes: While both methods can yield moderate to high GI results, the way potatoes are cooked matters. Boiled potatoes generally have a lower GI than baked potatoes, especially when cooled after boiling, as this can increase the resistant starch content. French fries, with their high surface area and often fried in oil, tend to have a very high GI.
- Grain Cooking: How long grains like rice or quinoa are cooked can also affect their GI. Longer cooking times can lead to a higher GI.
Combination of Foods
The GI of a meal is a composite of all the foods consumed. Combining carbohydrate-rich foods with protein, fat, and fiber can significantly lower the overall glycemic response of the meal.
- Adding Protein and Fat: Including sources of protein (like chicken, fish, or beans) and healthy fats (like avocado or olive oil) alongside carbohydrate-rich foods helps to slow down digestion and absorption, thereby moderating blood sugar spikes. For instance, having toast with avocado or eggs will have a lower GI than eating plain toast.
- Adding Fiber: Foods high in fiber, such as vegetables and legumes, are excellent additions to meals to lower the overall GI. A meal of pasta with a rich vegetable sauce will have a lower GI than plain pasta.
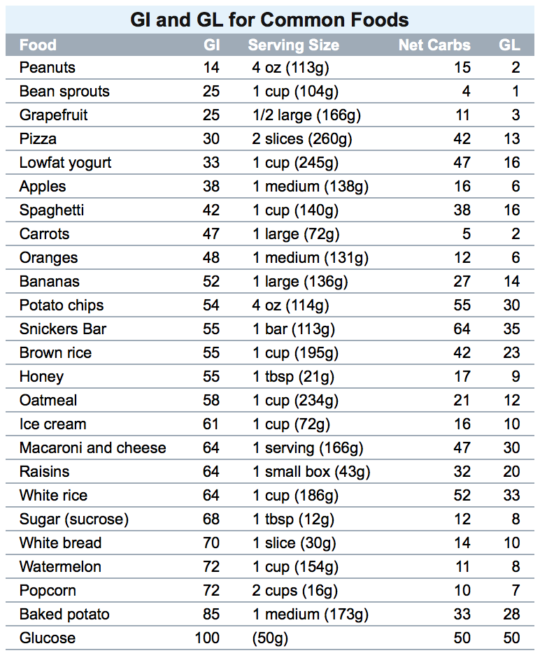
The Glycemic Load: A More Comprehensive Measure
While the glycemic index (GI) is a useful tool, it has limitations. It only considers the quality of carbohydrates and not the quantity consumed. This is where the glycemic load (GL) comes into play, offering a more practical and comprehensive picture of a food’s impact on blood sugar.
Understanding Glycemic Load (GL)
The glycemic load takes into account both the GI of a food and the amount of carbohydrate in a typical serving. It is calculated using the following formula:
Glycemic Load (GL) = (Glycemic Index (GI) / 100) * Grams of Carbohydrates per Serving
Like the GI, the GL is also categorized into three levels:
- Low GL (10 or less): Foods with a low GL have a minimal impact on blood sugar levels.
- Medium GL (11-19): Foods with a medium GL have a moderate impact on blood sugar.
- High GL (20 or more): Foods with a high GL can cause significant spikes in blood sugar.
Why GL is Often More Practical
The GL provides a more realistic assessment of how a food will affect your blood sugar because it considers the actual amount of carbohydrates you are likely to eat. For example, watermelon has a relatively high GI (around 76), which might make it seem like a food to avoid. However, a typical serving of watermelon contains relatively few carbohydrates. Therefore, its GL is quite low (around 4). This means that while watermelon does raise blood sugar quickly, the overall effect on your blood sugar from a standard portion is minimal.
Conversely, a food with a moderate GI but a very high carbohydrate content per serving can still have a high GL and a significant impact on blood sugar. For instance, while brown rice has a moderate GI (around 50-60), a large serving can result in a high GL.
Using GL in Dietary Planning
When planning meals, considering the GL alongside the GI offers a more nuanced approach.
- Prioritize Low GL Foods: Aim to build your diet around foods with a low GL. This includes most non-starchy vegetables, fruits (in reasonable portions), legumes, and moderate amounts of whole grains and lean proteins.
- Moderate Portions of Medium GL Foods: Foods with a medium GL can be enjoyed as part of balanced meals, especially when paired with low-GL foods, protein, and healthy fats to mitigate their impact.
- Limit High GL Foods: High GL foods should be consumed sparingly. These are typically found in highly processed items, sugary beverages, and large portions of refined grains and starchy foods.
By understanding and applying the concept of glycemic load, individuals can make more informed food choices that better support stable blood sugar levels and overall metabolic health.
Practical Strategies for a Low-Glycemic Diet
Adopting a low-glycemic eating pattern doesn’t require restrictive dieting. It’s about making smart, consistent choices that prioritize nutrient-dense, slowly digested carbohydrates. Here are practical strategies to help you incorporate low-GI principles into your daily life:
Building Balanced Meals
The foundation of a successful low-GI diet is building meals that combine various food groups for sustained energy and satiety.
- Start with Non-Starchy Vegetables: Make vegetables the centerpiece of your plate. They are packed with fiber, vitamins, and minerals, and have a minimal impact on blood sugar. Aim to fill at least half your plate with colorful vegetables like leafy greens, broccoli, cauliflower, bell peppers, and zucchini.
- Include Lean Protein: Protein sources help to slow down digestion and increase feelings of fullness. Opt for lean meats, poultry, fish, eggs, tofu, tempeh, and legumes. A palm-sized portion of protein at each meal is a good guideline.
- Add Healthy Fats: Healthy fats also contribute to satiety and slow down carbohydrate absorption. Incorporate sources like avocados, nuts, seeds, and olive oil into your meals. A small amount of healthy fat can make a significant difference in your blood sugar response.
- Choose Low-GI Carbohydrate Sources Wisely: When including carbohydrates, prioritize whole, unprocessed options. This includes:
- Whole Grains: Quinoa, barley, oats, buckwheat, and brown rice.
- Legumes: Lentils, chickpeas, black beans, and kidney beans.
- Certain Fruits: Berries, apples, pears, oranges, and stone fruits.
- Sweet Potatoes: In moderation.
Smart Snacking Choices
Snacking between meals can be a pitfall for blood sugar management if not done thoughtfully. Opting for low-GI snacks can prevent energy dips and overeating at main meals.
- Fruits with Nuts or Seeds: An apple or pear paired with a small handful of almonds or walnuts provides fiber, protein, and healthy fats for a balanced snack.
- Vegetables with Hummus or Guacamole: Carrot sticks, cucumber slices, or bell pepper strips dipped in hummus or guacamole offer fiber and healthy fats.
- Yogurt with Berries: Unsweetened Greek yogurt topped with a handful of fresh berries is a protein-rich, low-GI option.
- Hard-Boiled Eggs: A convenient and portable source of protein.
- Edamame: Steamed edamame pods are a good source of protein and fiber.
Reading Labels and Understanding Ingredients
Becoming a savvy consumer involves understanding food labels and ingredient lists to make informed choices.
- Look for “Whole Grain” as the First Ingredient: On bread, pasta, and cereal products, ensure “whole wheat,” “whole oats,” or another whole grain is listed as the first ingredient. Avoid products where refined grains like “enriched flour” or “white flour” are primary.
- Beware of Added Sugars: Many processed foods, even those marketed as healthy, contain significant amounts of added sugars, which contribute to a higher GI. Look for sugar in various forms, such as corn syrup, fructose, dextrose, sucrose, and maltose.
- Fiber Content: Higher fiber content generally correlates with a lower GI. Aim for products with at least 3 grams of fiber per serving.
- Glycemic Index Charts and Apps: Utilize readily available online resources and mobile applications that provide GI values for common foods. These tools can be invaluable for meal planning and grocery shopping.

Hydration and Portion Control
Staying adequately hydrated and practicing mindful portion control are essential complements to a low-GI eating plan.
- Water is Key: Drink plenty of water throughout the day. Sometimes thirst can be mistaken for hunger, leading to unnecessary snacking.
- Mindful Eating: Pay attention to your body’s hunger and fullness cues. Eat slowly, savor each bite, and stop when you feel comfortably satisfied, not overly full.
- Appropriate Serving Sizes: Be mindful of portion sizes, especially for carbohydrate-rich foods. Even low-GI carbohydrates can contribute to a higher glycemic load if consumed in excessive quantities. Using smaller plates and measuring cups can be helpful.
By implementing these practical strategies, individuals can effectively navigate their dietary choices, focusing on foods that promote stable blood sugar, sustained energy, and long-term health benefits.
